- Visibility 372 Views
- Downloads 35 Downloads
- DOI 10.18231/j.ijmpo.2024.025
-
CrossMark
- Citation
Combined in–office and at-home bleaching of vital teeth in an adolescent patient- A case report
Introduction
Patients with dental fluorosis typically have a history of prolonged excessive fluoride intake during the crucial period of enamel formation, from birth to approximately eight years of age. The severity of dental fluorosis varies widely, ranging from subtle white opaque spots that are less noticeable to more prominent pitting and discoloration of the enamel, which can result in dark yellow brown discolorations as well. [1]
While fluoride is essential for bone and tooth health, as it combines with calcium to form hydroxyapatite and strengthens calcified tissues, excessive intake over time can lead to dental fluorosis, skeletal fluorosis, and even reduced intelligence in children. High rates of dental fluorosis among adolescents are a growing concern, particularly due to the potential psychological impact. Discoloured and porous enamel can be aesthetically unsatisfactory, negatively affecting a child’s self-esteem and social interactions. [2]
The World Health Organization (WHO) has set the maximum fluoride concentration in drinking water at 1.5 mg/L to prevent fluorosis. In 2008-09, National Program for Prevention and Control of Fluorosis (NPPCF) was initiated by India in response to that. This program identifies areas with elevated fluoride levels, manages water sources, and screens schools and communities for fluorosis. It encompasses comprehensive case management, ensuring drinking water quality meet standards, and improving children's nutrition to mitigate fluorosis effects. [3]
For children with dental fluorosis, there are several cosmetic treatments available. To restore the natural white appearance of enamel, tooth can be bleached, whitened, and micro-abrasion or macro-abrasion can remove subsurface porosities and extrinsic stains. When porosities are too deep for micro-abrasion without causing sensitivity or altering tooth shape, veneering the enamel surface with porcelain or resin composite can enhance aesthetics. [4] In young children and adolescents less invasive procedures like bleaching is generally the preferred choice of treatment.
The aesthetic appeal of a smile is of great importance. Tooth whitening, or bleaching is a popular non-invasive aesthetic procedure, first began for non-vital teeth in 1848 with chloride of lime. [5] Later, in 1864, Truman introduced a highly effective method for bleaching non-vital teeth, which involved releasing chlorine from a mixture of calcium hypochlorite and acetic acid. [6] Bleaching is frequently used to fully or partially restore discoloured teeth. It has always been and is the most popular aesthetic technique, due to its low cost, non-invasive nature, and conservative approach. [7]
The history of vital tooth bleaching dates to 1868 with the introduction of oxalic acid, followed by using Pyrozone in 1892. In 1911, hydrogen peroxide became the standard bleaching agent in dental clinics, often activated by heat or light. In the 1960s, Dr. Bill Klusmier pioneered a successful at-home bleaching method using Gly-Oxide, a 10% carbamide peroxide oral antiseptic, administered with a custom-fitted mouth tray. This method improved both gingival health and tooth color. Subsequently, Gly-Oxide was replaced by Proxigel, a 10% carbamide peroxide formulation with a slower release, specifically designed for orthodontic patients. This modification enhanced both the effectiveness and convenience of the bleaching process. [8]
Tooth bleaching can be divided into three main types: internal or nonvital, external or vital, and at-home bleaching. Internal bleaching process places the bleaching agent inside the tooth that has undergone endodontic treatment, either through direct application by a dentist or the "walking bleach" technique, where the bleaching agent is placed in the tooth and left between appointments. [3] External bleaching, involves applying the bleaching agent on the enamel surface of a tooth with healthy pulp, and includes at-home bleaching, in-office bleaching, and over-the-counter products. At-home bleaching involves the patient using custom-fitted custom-fitted trays either provided by by a dentist or over the counter products the counter products like tooth whitening pastes which vary in strength and effectiveness compared to professional treatments. [9] The success of these methods depends on the ability of the bleaching agents, usually peroxides, to penetrate the enamel and dentin, breaking down stains and whitening the teeth.
Stains can also be classified into extrinsic and intrinsic stains. Extrinsic stains occur on external tooth surface due to the accumulation of chromatogenic substances from consumption of stain-causing foods and drinks, or tobacco use and poor oral hygiene. These stains are primarily localized in the pellicle either because of reactions between sugars and amino acids or due to the retention of external chromophores. Intrinsic stains are typically due to internal discoloration or defects in the enamel caused by aging, consumption of stain-inducing foods and beverages, tobacco use, enamel microcracks, tetracycline antibiotics, high fluoride intake, severe jaundice in infancy, porphyria, dental decay, restorations, and the natural thinning of the enamel layer.[8] Fluorosis is a very common public health problem is India especially in certain belts like in Orissa, Karnataka to name a few where adolescent school goers show considerable dental staining due to ingested fluorides through food and drinking water. [10]
In-office bleaching is a type of vital bleaching technique utilizing hydrogen peroxide, in varying concentrations often enhanced with agents like titanium dioxide activated by light or heat for a period of 15-30 minutes. [11] Hydrogen peroxide may be mixed with titanium dioxide or nitrogen-doped titanium dioxide to act as a photocatalyst, activated by a specialized light or laser for faster results. [12]
Case Report
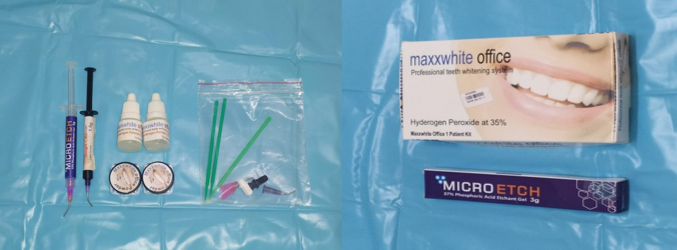
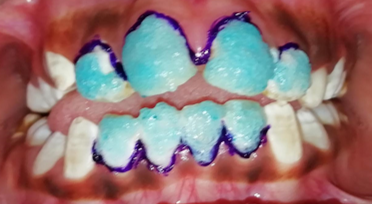
A twelve-year-old male patient was referred to the Department of Pedodontics and Preventive Dentistry in Kalinga Institute of Dental Sciences with the complaint of discoloration of teeth. His clinical history was recorded, intra-oral examination was done for caries, [13] and other findings and a diagnosis of fluorosis was reached. On intra-oral examination noticeable brown/yellow staining of his teeth was observed. Mild to moderate fluorosis staining was diagnosed on the anterior and posterior teeth based on Dean's Fluorosis Index. His parents desired for the least invasive and cost-effective management of the condition. Thus, it was decided instead of other aesthetic treatments available like veneers, in-office vital bleaching would be done. Clinical photographs were taken before starting of the procedure. ([Figure 1], [Figure 2]) For this patient, 35% hydrogen peroxide, Maxx white Office® was selected as the bleaching agent. ([Figure 3]) In-office bleaching is a clinically safe and effective whitening procedure to enhance the whitening effect using hydrogen peroxide concentrations, typically between 30% and 35%, helping in reducing sensitivity.[14] A liquid dam was applied as a barrier and cured for gingival protection. ([Figure 4]) Bleaching agent and powder were mixed in equal parts and the homogenous, thick mix prepared was applied uniformly on the tooth surfaces using an applicator tip and left for 20 minutes. ([Figure 5]) Then the homogenous mix was washed off using air-water syringe. This process was repeated again during the same visit. Post operative photographs were recorded ([Figure 6]).
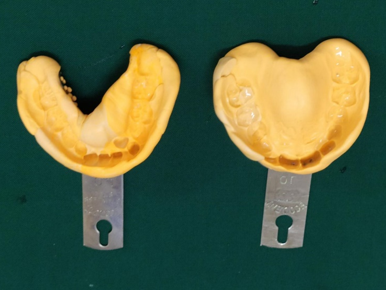
An impression was recorded of the upper and lower jaw for fabrication of custom-made trays for application of home bleach using elastomeric putty. ([Figure 7]) Custom made trays ([Figure 8]) were prepared and given to the patient for loading home bleach ([Figure 9]) and to be applied once a day for 10 days. Patient was recalled for second ([Figure 10], [Figure 11]) and third visits ([Figure 12], [Figure 13]) after a period of 1 month each and the same steps were repeated. Post operative photographs were recorded after each visit. White mottled enamel hypo-mineralisation with the most significant staining were visible on the maxillary anterior teeth especially tooth nos. 11 and 21 had dark brown streaks in the middle third of the facial surfaces at the beginning of the treatment which was found to significantly reduced by the third visit.










Discussion
Office bleaching, which utilizes high concentrations of hydrogen peroxide, is a highly effective method for enhancing tooth shade, capable of improving it by up to four grades. This effectiveness is notably increased with the use of photoactivation methods that enhance the bleaching outcome. [15] Despite its efficacy, the procedure presents certain challenges. Office bleaching can reduce enamel bonding performance due to changes in enamel porosity, even following phosphoric acid etching. [16] Additionally, it may cause temporary dehydration of the enamel, creating a misleading whitening effect until the enamel rehydrates, which necessitates final colour assessments to be conducted after a week. [17] Comparative studies, particularly those using split-mouth designs, indicate that office bleaching generally surpasses home methods in both whitening effectiveness and longevity. [18] However, it often results in moderate tooth sensitivity immediately after treatment due to the rapid penetration of hydrogen peroxide, potentially leading to inflammatory reactions in the tooth. Sensitivity levels reported across studies vary; some suggest higher sensitivity with in-office treatments, while others find greater sensitivity with home techniques. [19] These differences are frequently attributed to variations in agent concentrations and whether desensitizing components are included to maximize the benefits of bleaching while minimizing risks, it is recommended that professionals adhere to manufacturer protocols, carefully balance hydrogen peroxide concentration with application duration, and consider a combination of in-office and at-home treatments for sustained, lower-risk whitening. This combined approach, coupled with individualized treatment plans that protect soft tissues and consider patient-specific factors such as sensitivity and enamel thickness, ensures that the whitening benefits of office bleaching are achieved without compromising enamel health. [20]
In aesthetic rehabilitation, the goal is to enhance the patient's appearance and boost self-confidence while preserving tooth structure as much as possible. Treatment plans for enamel hypo-mineralization can vary widely based on the severity of the defect, with conservative approaches typically involving interventions like tooth bleaching, enamel macro-abrasion, micro-abrasion, and resin infiltration. [21] A recent clinical report recommends treating enamel fluorosis stains with at-home bleaching using a 10% carbamide peroxide gel in an overnight tray as the initial step, followed by resin infiltration to conceal residual white spots. [22] In contrast, in this case, in-office bleaching was chosen to ensure compliance, as the patient's likelihood of wearing an overnight tray was uncertain. Additionally, in-office bleaching did not lead to sensitivity in this case. [23]
In preparation for in-office bleaching, the dentist first examines the teeth to ensure there are no caries, gingival complications, or other dental concerns that could complicate the procedure. Once confirmed, a protective barrier, typically a gel or rubber shield, is applied to the gingiva to shield them from the bleaching agent following which a high concentration of hydrogen peroxide or carbamide peroxide is applied directly to the teeth, where it penetrates the enamel to target discoloured areas within. Some in-office treatments also incorporate a specialized light or laser, which can activate or accelerate the bleaching process, intensifying the whitening effect which was not done in this case. This step is optional and varies depending on the system used by the dentist. The bleaching agent is generally left on the teeth for 15-30 minutes before being rinsed off. This process is often repeated multiple times in a single session to achieve the desired level of whiteness. While significant results are often visible after one session, additional appointments may occasionally be recommended for optimal results. [23], [24]
In-office bleaching offers several advantages that make it a popular choice for treatment of fluorosis and those seeking immediate and effective tooth whitening. One of the key benefits is the speed of results; in-office treatments often deliver noticeable whitening after just one visit, lightening teeth by several shades within a short time. Another advantage that can be listed here is the extent of customization possible. It is a cost-effective, non-invasive, and conservative procedure.
Conclusion
Dentists can customize the concentration of the bleaching agent and adjust the number of applications to meet each patient’s needs, ensuring a balance between whitening effectiveness and sensitivity. Professional supervision enhances the safety of the procedure, as in-office bleaching occurs in a controlled environment. This reduces the risk of gingival irritation or enamel damage, and the dentist can make real-time adjustments if discomfort arises. [8] The combination of immediate results, personalized treatment, and safety makes in-office bleaching a reliable choice. It is essential to follow post-treatment care instructions to maintain the results, such as avoiding stain-causing foods and drinks like coffee, tea, and tobacco for 24-48 hours, and practicing good oral hygiene through regular brushing, flossing, and cleanings. [25] This patient was followed up for 3 months and visible changes were observed in this case through vital bleaching procedure.
Conflict of Interest
None.
Source of Funding
None.
References
- MM Patil, BB Lakhkar, SS Patil. Curse of fluorosis. Indian J Pediatr 2018. [Google Scholar]
- A Verma, BK Shetty, V Guddattu, MK Chourasia, P Pundir. High prevalence of dental fluorosis among adolescents is a growing concern: a school based cross-sectional study from Southern India. Environ Health Prev Med 2017. [Google Scholar] [Crossref]
- ES Akpata. Therapeutic management of dental fluorosis: A critical review of literature. Saudi J Oral Sci 2014. [Google Scholar]
- Z Daskalaki, E Alifakioti, A Arhakis. Aesthetic treatment of dental fluorosis in a 9-year-old girl: Case Report. Balkan J Dent Med 2019. [Google Scholar]
- WW Dwinelle. Ninth annual meeting of American Society of Dental Surgeons: article X. Am J Dent Sci 1850. [Google Scholar]
- EC Kirk. . Hints, queries, and comments 1906. [Google Scholar]
- M Gupta, J Kalotra, M Mall, S Targotra, P Gupta, Anukriti. Dental Bleaching: An Overview. Asian Pac J Health Sci 2020. [Google Scholar]
- MQ Alqahtani. Tooth-bleaching procedures and their controversial effects: A literature review. Saudi Dent J 2014. [Google Scholar]
- C Bersezio, P Ledezma, C Mayer, O Rivera, OB Junior, E Fernández. Effectiveness and effect of non-vital bleaching on the quality of life of patients up to 6 months post-treatment: a randomized clinical trial. Clin Oral Investig 2018. [Google Scholar]
- A Verma, BK Shetty, V Guddattu, MK Chourasia, P Pundir. High prevalence of dental fluorosis among adolescents is a growing concern: a school based cross-sectional study from Southern India. Environ Health Prev Med 2017. [Google Scholar] [Crossref]
- TG Savian, J Oling, FZ Soares, RO Rocha. Vital Bleaching Influences the Bond Strength of Adhesive Systems to Enamel and Dentin: A Systematic Review and Meta-Analysis of In Vitro Studies. Oper Dent 2021. [Google Scholar]
- BM Maran, T De Paris Matos, AD De Castro, L Vochikovski, AL Amadori, AD Loguercio. In-office bleaching with low/medium vs. high concentrate hydrogen peroxide: A systematic review and meta-analysis. J Dent 2020. [Google Scholar] [Crossref]
- AM Moldovan, V Popescu, CV Ionescu, S Cuc, A Craciun, M Moldovan. Various Aspects Involved in the Study of Tooth Bleaching Procedure: A Questionnaire-Based Study. Int J Environ Res Public Health 2022. [Google Scholar] [Crossref]
- S Dutta, A Mohapatra. Early childhood caries- Etiology, prevention and management: A Review. Arch Dent Res 2022. [Google Scholar]
- JJ Nugroho, NP Putri. Interdisciplinary treatment in office bleaching for discoloration teeth with altered passive eruption: a case report. Makassar Dent J 2022. [Google Scholar]
- S Halabi, N Matsui, T Nikaido, MF Burrow, J Tagami. Effect of Office Bleaching on Enamel Bonding Performance. J Adhes Dent 2019. [Google Scholar]
- A Mounika, J Mandava, B Roopesh, G Karri. Clinical evaluation of color change and tooth sensitivity with in-office and home bleaching treatments. Indian J Dent Res 2018. [Google Scholar]
- LS Machado, RB Anchieta, PH Santos, AL Briso, N Tovar, MN Janal. Clinical Comparison of At-Home and In-Office Dental Bleaching Procedures: A Randomized Trial of a Split-Mouth Design. Int J Periodontics Restorative Dent 2016. [Google Scholar]
- SH Donassollo, TA Donassollo, S Coser, S Wilde, JLS Uehara, LA Chisini. Triple-blinded randomized clinical trial comparing efficacy and tooth sensitivity of in-office and at-home bleaching techniques. J Appl Oral Sci 2021. [Google Scholar] [Crossref]
- M Aidos, C M Marto, I Amaro, M Cernera, I Francisco, F Vale. Comparison of in-office and at-home bleaching techniques: An umbrella review of efficacy and post-operative sensitivity. Heliyon 2024. [Google Scholar] [Crossref]
- M Kury, EE Wada, DPD Silva, CPM Tabchoury, M Giannini, V Cavalli. Effect of violet LED light on in-office bleaching protocols: a randomized controlled clinical trial. J Appl Oral Sci 2020. [Google Scholar] [Crossref]
- J Perdigão, VQ Lam, BG Burseth, C Real. Masking of Enamel Fluorosis Discolorations and Tooth Misalignment With a Combination of At-Home Whitening, Resin Infiltration, and Direct Composite Restorations. Oper Dent 2017. [Google Scholar]
- Z Aboelenein, MI Riad, MF Haridy. Case Report: In-office bleaching, microabrasion, and resin infiltration for the correction of hypomineralized esthetic defects. F1000Research 2019. [Google Scholar] [Crossref]
- LB He, MY Shao, K Tan, X Xu, JY Li. The effects of light on bleaching and tooth sensitivity during in-office vital bleaching: a systematic review and meta-analysis. J Dent 2012. [Google Scholar]
- G Côrtes, NP Pini, DA Lima, PC Liporoni, E Munin, GM Ambrosano. Influence of coffee and red wine on tooth color during and after bleaching. Acta Odontol Scand 2013. [Google Scholar]
How to Cite This Article
Vancouver
Dutta S, Palla G, Dutta B, Mohapatra A. Combined in–office and at-home bleaching of vital teeth in an adolescent patient- A case report [Internet]. IP Int J Med Paediatr Oncol. 2024 [cited 2025 Sep 13];10(4):97-102. Available from: https://doi.org/10.18231/j.ijmpo.2024.025
APA
Dutta, S., Palla, G., Dutta, B., Mohapatra, A. (2024). Combined in–office and at-home bleaching of vital teeth in an adolescent patient- A case report. IP Int J Med Paediatr Oncol, 10(4), 97-102. https://doi.org/10.18231/j.ijmpo.2024.025
MLA
Dutta, Sharbari, Palla, Gayatri, Dutta, Brahmananda, Mohapatra, Abinash. "Combined in–office and at-home bleaching of vital teeth in an adolescent patient- A case report." IP Int J Med Paediatr Oncol, vol. 10, no. 4, 2024, pp. 97-102. https://doi.org/10.18231/j.ijmpo.2024.025
Chicago
Dutta, S., Palla, G., Dutta, B., Mohapatra, A.. "Combined in–office and at-home bleaching of vital teeth in an adolescent patient- A case report." IP Int J Med Paediatr Oncol 10, no. 4 (2024): 97-102. https://doi.org/10.18231/j.ijmpo.2024.025
