Introduction
SARS-CoV-2 is a new virus that is responsible for COVID-19, a global pandemic that has already claimed the lives of almost half a billion people. SARS CoV-2 is known to cause gastrointestinal problems in children like diarrhea, vomiting, abdominal pain, hepatitis, pancreatitis1 etc. Here we report a novel case of SARS CoV-2 virus causing acute severe ileocolitis in a 14-year-old child. Diffuse inflammatory infiltrates of the submucosa of a segment of the intestine characterize the inflammation of the alimentary tract.2 The inflammatory response could spread to the serosal membrane and Peritonitis, or septicemia may also develop post infection with the virus.3
Case Presentation
A 14-year-old previously healthy child presented to pediatric OPD with complaints of on and off abdominal pain for 2 weeks. Diffuse, dull-aching intermittent pain, mild to moderate in intensity, 3-4 episodes per day, each episode lasting for 5-10 minutes, aggravated after having food. No fever. No nausea. No vomiting. No loose stools. No H/O burning micturition. No chronic cough. No H/O gastrointestinal disease or weight loss. On clinical examination child was afebrile, temperature 98⁰F, RR-18/min, PR- 84/min, BP-110/70 mm, SpO2-99%. Child was conscious and alert. There was no throat congestion, no lymphadenopathy, no edema. The heart rate and rhythm were normal. Normal vesicular breath sounds heard bilaterally without added sounds. The abdomen was soft, not distended, non-tender, no organomegaly. The clinical possibilities considered were chronic appendicitis, chronic pancreatitis, abdominal tuberculosis, viral hepatitis, enterocolitis and COVID infection.
Evaluation during hospitalization
Blood work revealed evidence of inflammation including elevated C-reactive protein, erythrocyte sedimentation rate, procalcitonin, d-dimer, ferritin, and neutrophils, and reduced lymphocyte. Infectious evaluation was positive for COVID-19.
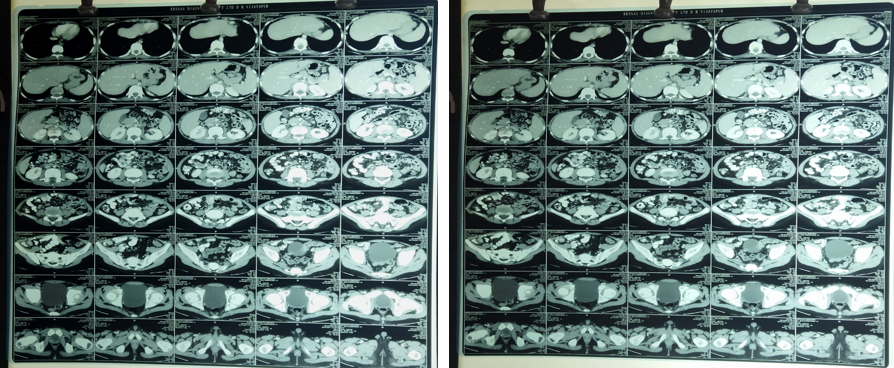
The initial investigations were as follows-Total leukocyte count-8980, neutrophils-69%, lymphocytes- 18%, platelet count-5.3 lakh, hemoglobin-8.8, PCV-28.8, CRP-16.9(>10-positive), D-Dimer-279, COVID- IgM and IgG- Positive. IgM- 2.5 and IgG- 1.8 (>1 Positive), HIV, HBsAg- negative, urine routine-normal. Peripheral smear showed microcytic hypochromic anemia with thrombocytosis. CBNAAT of gastric aspirate was done to rule out abdominal tuberculosis- reported negative. Chest x-ray was normal. USG abdomen and pelvis showed caecum and terminal ileal loop wall thickening and adjacent mesenteric lymphadenopathy, possibly enterocolitis. CT scan of abdomen showed diffuse wall thickening of right ileocolic junction and distal ileum with adjacent discrete lymph nodes.
Table 1
Laboratory results
Treatment
Considering the clinical findings, blood investigation reports and ultrasonography findings, child was treated with intravenous fluids maintenance and intravenous ofloxacin and metronidazole injection for 5 days. Child was also started on steroids, Tab. prednisolone 2mg/kg/day was given for 2 weeks. After the initiation of steroids child showed improvement and got discharged on 8th day. Child was asymptomatic at 2 weeks follow-up visit.
Discussion
Inflammation of the alimentary tract is a unique presentation of the novel SARS-CoV-2 virus. Historically, this inflammation is hypothesized to be of bacterial origin, but its portal of entry and the pathogenesis remains unclear.3 Our patient did not report any chronic gastrointestinal symptoms, and stool studies were also normal. Mimics of inflammatory bowel disease (IBD) include not only infectious causes of colitis, but also vascular diseases, radiation-related injuries, drug induced inflammation, and monogenic disorders in very-early-onset refractory IBD. A superinfection with cytomegalovirus or Clostridium difficile can aggravate intestinal inflammation in IBD, especially in patients who are immunocompromised. 4 Our patient had a negative comprehensive infectious evaluation (Table 1), except for positive COVID-19 IgM and IgG which indicated a COVID infection that lead to the presentation. This case highlights the rare presentation of COVID-19 in which child presented only with on and off abdominal pain and was diagnosed as COVID-19 associated ileo colitis.
The SARS-CoV-2 virus is an enveloped, single-stranded virus, and the angiotensin-converting enzyme 2 (ACE2) receptor is considered as the major receptor for the viral spike protein and critical for infectivity.2 The ACE2 protein is found at high levels in the colon, biliary system, and liver, and viral RNA shedding occurs in the GI tract.4 These data indicates that the SARS-CoV-2 may have tropism for the GI tract and liver, and they can be the sites of active viral replication causing either direct or indirect tissue injury.4
Conclusion
COVID-19 added another dimension to gastro-intestinal diseases. The primary clinical manifestation of COVID-19 infection in children is not necessarily a pulmonary disease in all cases. The involvement of multiple organ systems, including the gastrointestinal (GI) tract, liver, and pancreas are also common.3 This is one of the rare, reported case of ileocolitis secondary to asymptomatic COVID-19 infection. It is prudent for pediatricians and pediatric gastroenterologists during the COVID-19 era to be aware of this unique presentation of the novel virus to avoid unnecessary invasive surgical intervention in cases of acute abdomen presentation in children. Given the ongoing emergency of GI manifestations of the disease, a high index of suspicion should be kept for COVID-19 in all children presented with GI symptoms.