Introduction
Hyperbilirubinemia is one of common problems seen in neonates requiring admission for phototherapy.1 Serum bilirubin concentration exceeding 5-7mg% causes neonates to appear clinically icteric.2
Jaundice is the commonest abnormal clinical finding in neonates.3 The average incidence of neonatal jaundice in India, as reported in several publications, is around 54.6% to 77%.4 Jaundice occurs when the immature neonatal liver is unable to clear a sufficient amount of bilirubin from the plasma.5 Yellowish discoloration of the skin is the result of accumulation of unconjugated lipid-soluble bile pigment.6
Pathological jaundice is known to occur in 4-8% of newborns.7 The common causes include blood group incompatibilities, prematurity, G6PD deficiency and sepsis with majority being idiopathic. Other less common causes include Infants of diabetic mothers, cephalhematoma and polycythemia.8 The immature brain of the newborn is susceptible to unconjugated bilirubin toxicity resulting in the acute manifestation, BIND.9
Assessment of jaundice should be done in the natural light. The pulp of the finger or thumb is pressed into the baby’s skin, preferably over a bony part till it blanches and underlying skin is noted for the yellow discoloration.
The criteria for intervention to control hyperbilirubinemia vary in different clinical situations, and on gestational age of the infants. Intervention for neonatal jaundice is based on guidelines for phototherapy and exchange transfusion for infants more than 35 weeks of gestation as published by the American Academy of pediatrics.10 Phototherapy is a cheap, effective and safe method of management of neonatal hyperbilirubinemia.11
The present study will try to analyze the causes, risk factors, both maternal and neonatal, and clinical profile of neonates admitted with hyperbilirubinemia.
Materials and Methods
The present study was conducted at NICU, Department of Pediatrics, Princess Esra hospital, Deccan Medical College, Hyderabad, India, from October 2019 to October 2020. A written informed consent was obtained from all parents of the babies involved in this study.
Selection of cases
The babies delivered at the hospital as well as babies referred from other hospitals of age 0-28 days during a period of one-year duration were included in this study. Late pre term and full-term babies, both healthy and sick, were included.
Sample size
Comprised of 210 neonates with jaundice (serum bilirubin more than 12mg/dl) hospitalized in the neonatal unit in Princess Esra hospital during the study period.
Methods
Jaundice was identified and assessed by clinical methods and confirmed by biochemical methods. Jaundice was clinically estimated by Kramer’s rule in broad daylight and confirmed by Serum bilirubin. Detailed antenatal, natal and postnatal history was taken. Clinical risk factors for jaundice were documented for every baby, and a detailed neurological examination including BIND score was performed for all babies requiring treatment for jaundice. A basic evaluation for cause for hyperbilirubinemia (CBP, Reticulocyte count, G6PD and DCT) was done in babies with Serum bilirubin levels more than 18mg/dl.
Serum Bilirubin measurement estimation was done via Van den Bergh method. Only those babies having serum bilirubin concentration of more than 12 mg/dl were included in the study.
Babies were treated according to guidelines published by American Academy of Pediatrics charts with phototherapy and/or exchange transfusion. Serum bilirubin levels were monitored periodically. The neonates were treated according to standard guidelines and monitored throughout their stay in the hospital. The side effects of phototherapy and/or DVET were documented during NICU stay.
Results
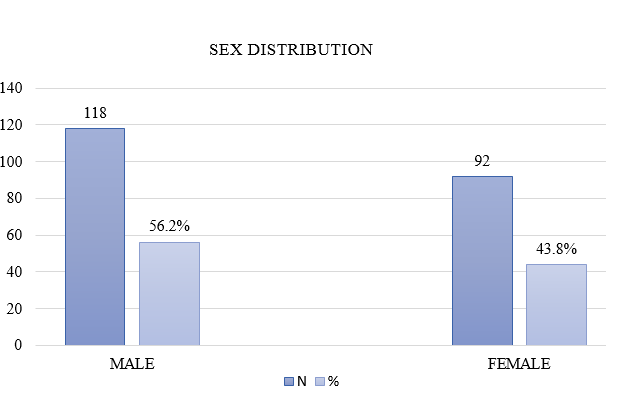
In this study of 210 neonates, 118 (56.20%) were male while 92 (43.80%) neonates were female as shown in Figure 1.
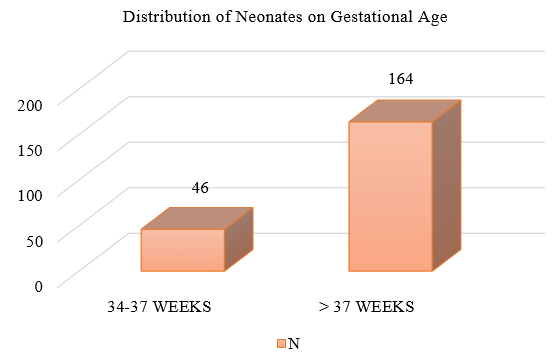
Out of 210 neonates studied, 46 (21.90%) were of 34-37 weeks gestational age and 164 (78.10%) were of more than 37 weeks gestational age as shown in Figure 2.
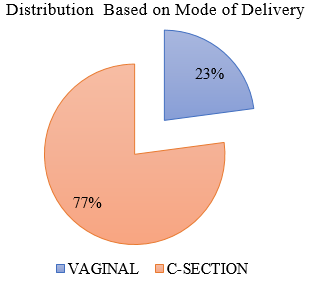
Out of 210 neonates, 48 (22.96%) were born via vaginal delivery while 162 (77.14%) neonates were delivered via Caesarean section as shown in Figure 3.
Table 1
Distribution according to Birth weight
|
S.No |
Weight (Grams) |
Frequency |
Percentage |
|
1. |
1000-1500 |
2 |
0.95% |
|
2. |
1501-2000 |
18 |
8.57% |
|
3. |
2001-2500 |
55 |
26.19% |
|
4. |
2501-3000 |
97 |
46.19% |
|
5. |
>3000 |
38 |
18.10% |
|
|
Total |
210 |
100% |
In this study of 210 neonates, 2 (0.95%) were in the weight range of 1000-1500 grams, 18 (8.57%) neonates were between 1501-2000 grams, 55 (26.19%) neonates were in the 2001-2500 grams range, 97 (46.19%) neonates were in the 2501-3000 grams range and 38 (18.10%) neonates weighed more than 3000 grams as detailed in Table 1.
Table 2
Distribution based on birth weight
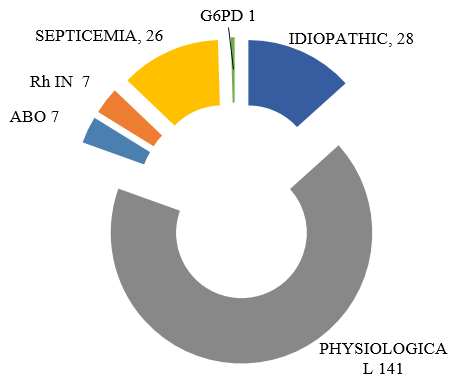
Fetal prematurity was found to be the most common risk factor followed by prolonged labor. Birth Asphyxia and PROM > 18 hours were the other risk factors noted behind the etiologies. as depicted in Table 2 . Considering the Etiology our study have ruled out that out of 210 Neonates studied, the etiology was Idiopathic Hyperbilirubinemia in 28 neonates, physiological hyperbilirubinemia seen in 141 neonates, ABO and Rh incompatibility was the cause in 7 neonates each, Septicemia was identified as the cause in 26 neonates and G6PD deficiency was the cause in 1 neonate. Physiological jaundice was taken as Serum Bilirubin levels less than 15mg/dl in well infants with no other risk factors for jaundice.
Table 3
Distribution Based on Sr. Bilirubin when starting Phototherapy
|
S. No |
Sr. Bilirubin level (mg/dl) |
Frequency |
Percentage |
|
1. |
12-15 |
125 |
59.5% |
|
2. |
15.1-18 |
42 |
20% |
|
3. |
18.1-20 |
21 |
10% |
|
4. |
>20 |
22 |
10.4% |
|
|
Total |
210 |
100% |
In this study of 210 neonates, at the time of starting phototherapy, 125 (59.52%) neonates had serum bilirubin between 12-15 mg/dl, 42 (20.00%) neonates had bilirubin values between 15.1-18 mg/dl, while 21 (10.00%) neonates had bilirubin values between 18.1-20 mg/dl and in 22 (10.48%) neonates serum bilirubin value was more than 20 mg/dl as shown in Table 3.
Table 4
Distribution of Neonates Based on Mode of Therapy
|
S.No |
Mode of Therapy |
Frequency |
Percentage |
|
1. |
Phto therapy Alone |
207 |
98.5% |
|
2. |
Exchange Transfusion and Photo Therapy |
3 |
1.43% |
|
Total |
210 |
100% |
|
From the 210 neonates included in this study, 207(98.57%) neonates were treated with phototherapy alone while 3(1.43%) neonates required both exchange transfusion and phototherapy as shown in Table 4. Rh incompatibility was the etiology behind all 3(1.43%) neonates requiring exchange transfusion. Intravenous immunoglobulin (IVIG) was not required, as babies were admitted with Bilirubin values in the exchange zones, and warranted an immediate exchange transfusion. Subsequently, there was no alarming rise in bilirubin levels and did not warrant IVIG therapy
Table 5
Complications Developed During Treatment.
|
Complications during phototherapy |
Number of patients |
|
Loose motions |
4 |
|
Rash |
3 |
|
Total |
7 |
|
Complications during exchange transfusion |
Number of patients |
|
Cardiac arrest |
0 |
|
Hypoglycemia |
0 |
|
Septicemia |
0 |
|
Total |
0 |
During phototherapy, 4 neonates developed loose stools while 3 neonates developed rashes. There were no complications seen during exchange transfusion for all 3 neonates as shown in Table 5.
In our study, the average BIND score for babies with Idiopathic pathological jaundice was 3, for ABO, Rh incompatibility and Septicemia the score was 2 and the average score for babies with Physiological jaundice and due to G6PD deficiency was 1. An average BIND score of 1.8 was thereby noted for the 210 neonates involved in this study as shown in Figure 4.
Discussion
Total of 210 neonates of neonatal hyperbilirubinemia were studied in detail
Sex distribution
Out of 210 neonates, 56.20% were males and 43.80% were females.
Narang et al 12 also found a male predominance in their studies with 56.2 cases of the male sex.
Gestational age
46 neonates from the 210 were pre-term with 21.90% incidence while 164 neonates having an incidence of 78.10% were more than 37 weeks. Singhal et al 13 have found prematurity as the second most common cause of hyperbilirubinemia in their studies. Narang et al 12 found jaundice in 47.9% out of 917 preterm babies.
Age at admission
From the 210 babies involved in this study, the average age of the babies at the time of admission for phototherapy was 5 days of life.
Birth weight
In our study, maximum number of neonates (97) were having birth weight between 2501-3000 grams. 2 (0.95%) neonates were below 1500 grams and 18 (8.57%) neonates were between 1501 and 2000 grams. 38 (18.10%) neonates had birth weight more than 3000 grams. Singhal et al 13 found in his study that one-fourth of neonates (29.16%) developing hyperbilirubinemia were with low birth weight.
Narang et al 12 concluded from their studies that the incidence of neonatal jaundice was three times higher in LBW babies compared to babies above 2500 grams.
In our study, 35.71% neonates were of low birth weight. It is mainly because of maternal under nutrition, poverty, underutilization of health services and illiteracy seen in the general area.
Risk factors
Maternal: In our study maximum number (19) of babies who developed jaundice had prolonged labor while 8 neonates had PROM more than 18 hours.
Fetal: In 30 neonates prematurity was the aggravating factor while 7neonates had birth asphyxia. Singhal et al 13 found prematurity as a cause for jaundice in 16.7% neonates. They have also found birth asphyxia as aggravating factor for hyperbilirubinemia in 12.1% cases out of which maximum were in idiopathic group. Our findings correlate with Singhal et al.13
Etiology
Physiological hyperbilirubinemia: In 141 neonates, the jaundice was physiological as it appeared between 48-96 hours and disappeared by 6-7 days in term and 10-12 days in preterm babies. Our findings are similar to Merchant et al 14 and the findings in their study.
Intervention with phototherapy was started at bilirubin levels of 12mg/dl as very often, parents do not report for close follow-up post discharge and often are referred late in the course of illness with pathological jaundice.
Idiopathic hyperbilirubinemia: In 28 (13.33%) neonates, the cause was unidentified and labelled as Idiopathic.Merchant et al 14 found idiopathic hyperbilirubinemia in 66% cases, Verma M. et al[15] found idiopathic in 35% cases, Singhal et al 13 found idiopathic as the cause in 34.4% cases while Narang et al 12 found it in 57.8% cases. Our findings are close to that of Verma M. et al[15] and Singhal et al. 13
Septicemia: In 26 (12.40%) neonates, septicemia was the cause for jaundice out of which 14 were preterm and 19 were term babies. Various aggravating factors like PROM (n=2), Prolonged labor (n=6), Prematurity (n=6) and Asphyxia (n=3) were seen.
Various laboratory investigations were suggestive of septicemia with total WBC count >15,000 and elevated CRP (>6) values. Blood culture was positive in 15 neonates. All the neonates were treated with appropriate antibiotics. Septicemia as a cause for hyperbilirubinemia was found in 8% neonates by Merchant et al, 14 in 11.6% neonates by Verma et al,[15] in 5.7% neonates by Singhal et al 13 and in 9.6% neonates by Narang et al. 12 Our findings are in accordance with Verma et al[15] and Narang et al. 12
Rh incompatibility: This was noted in 7 (3.33%) neonates. Direct Coomb’s test was positive in all these neonates. Other investigations revealed hemolytic picture on peripheral smear and high reticulocyte count. Rh incompatibility was found in 18.6% neonates by Merchant et al, 14 in 8.1% neonates by Singhal et al, 13 in 2.9% by Narang et al, 12 and in 9.6% by Verma M. et al.[15] Our findings are close to Narang et al. 12
ABO incompatibility: Incidence of ABO incompatibility was same as that of Rh incompatibility at 3.33%. Merchant et al 14 found ABO incompatibility in 22.6% neonates, Verma M. et al[15] found it in 22.6% and Singhal et al 13 in 14.3% neonates. Our findings are closest to Singhal et al. 13
G6PD deficiency: It was found in only one neonate. Baby developed jaundice between 48-72 hours. G6PD deficiency was found in 2.6% neonates by Merchant et al, 14 in 5.1% by Singhal et al 13 and in 3.4% neonates by Narang et al. 12 Our findings are closest to Merchant et al. 14 The prevalence of G6PD deficiency is uncommon in Southern India.
Therapeutic interventions
Out of the 230 neonates, 3 required exchange transfusion. All of these 3 neonates had Rh incompatibility. Exchange transfusion was done when the serum bilirubin concentrations were in the transfusion zone according to the AAP charts for exchange transfusion. None of the babies developed BIND. Other risk factors like birth asphyxia, septicemia, hypoglycemia and acidosis were also considered while deciding exchange transfusion.
Singhal et al.13 found in their study that the commonest etiology behind babies requiring exchange transfusion was Rh incompatibility followed by ABO incompatibility and G6PD deficiency. Narang et al 12 found that the most common cause was Idiopathic, followed by Septicemia and G6PD deficiency. Rest of the 207 neonates in our study received phototherapy alone. Phototherapy was started when serum bilirubin was more than 12 mg/dl and was given for 24, 48 or 72 hours.
Conclusion
Most common cause of neonatal hyperbilirubinemia was found to be Physiological followed by Septicemia and Idiopathic etiologies. Blood group incompatibilities were less common causes.
Photo therapy is a cheap and effective way to reduce bilirubin levels in neonatal jaundice.
Need for exchange transfusion has significantly reduced due to more awareness and cautiousness of treating pediatricians. Exchange transfusion is a safe procedure and should be considered when indicated, to decrease the incidence of BIND. 11