Introduction
The reported incidence of EA, with or without TEF, is 1:3500 live-born infants. The first description of EA with the typical form of tracheoesophageal fistula (EA-TEF) appeared in 1697 in the fifth edition of Thomas Gibson’s. "The Anatomy of Humane Bodies Epitomized". The history of the surgical treatment of EA-TEF is remarkable and covers 270 years linking the first description and the first survivor.1 The earliest clinical sign of EA-TEF is usually excessive salivation that results from pooling of secretions in the pharynx. Typically, the first feeding is followed by regurgitation, coughing and choking.
Case Report
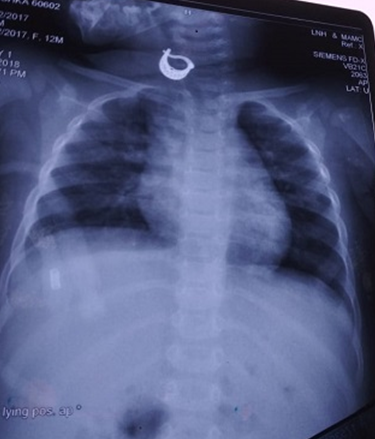
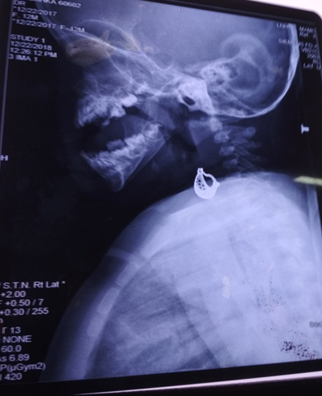
One and a half year old female child, a post op case of right posterolateral thoracotomy, ligation of TEF, cervical esophagostomy and feeding gastrostomy, awaiting definitive esophageal replacement surgery was brought to us with complaints of fever and runny nose. On examination baby was stable with pulse rate of 112/min, respiratory rate of 38/min and conducted sound were present on chest auscultation. The baby was treated with antihistaminics and antibiotics suspecting upper respiratory infection. After a week of therapy, the complaints persisted. Hence, a chest radiogram (CXR) was ordered which appeared grossly normal at the oversight with a radio opaque shadow away from tracheal air shadow along with infiltrates in the right lung field (Figure 1). This shadow was considered to be an artifact, probably the jewelry worn by the baby in neck. Otolaryngology consultation was also sought to rule out tonsillitis and adenoids. Indirect laryngoscopy was reported normal. Parents were advised to continue symptomatic treatment. Few days later, the child developed blood stained discharge from cervical esophagostomy. Repeat X-rays revealed the same shadow of the foreign body at the same place in various views, which compelled us to consider an alternate diagnosis. Repeat interview of the mother revealed that one of her earrings was missing for more than 3 weeks duration. Since child did not have significant respiratory distress and since the foreign body appeared outside the trachea (on the X-ray), we now considered the possibility of it being present in the esophageal pouch. Urgent esophagoscopy and retrieval of the upper pouch foreign body was done. Child improved gradually and recovered.
Discussion
The first successful repair of EA-TEF from India was reported by Professor Subir K. Chatterjee from Kolkatta in 1963. The survival rate of EA-TEF surgery is more than 90% in developed countries while survival rate in developing countries is far below.2 Factors responsible for this include home deliveries (which led to delayed diagnosis), improper perinatal care and poor transport facilty.
In most infants, open thoracotomy or thoracoscopic division of the fistula with primary anastomosis of the esophagus is possible and is the operative procedure of choice. Though in “long gap” cases, most pediatric surgeons proceed with the operative placement of a gastrostomy tube, a period of observation, and an attempted delayed primary repair or cervical esophagostomy with gastrostomy is done with esophageal replacement later on.
The ideal age of esophageal replacement may be between 6 months and 1 year. 2 The choice of esophageal substitute depends on many factors. Colon replacement, or ileocolon, has been used widely though gastric transposition has more recently become a well established and successful esophageal substitute in infants with EA. 1
It is important to stimulate the swallowing reflex by offering in sham oral feedings during regular gastrostomy feedings diverted TEF babies. Infants who achieve good sham-feeding undoubtedly rapidly accept oral nutrition when the esophageal substitute has been successfully connected.3 In our country, due to limited resources, the definitive esophageal replacement might be delayed in some babies till they become toddlers.
Foreign bodies in infants and toddlers are rare, though few cases of foreign body in neonates have been described.4, 5, 6, 7 In the present case, foreign body was found in upper pouch in a diverted TEF child. The foreign body ingestion is mostly accidental, though common complications associated with cervical esophagostomy are stricture and kinking of esophagus.8 To the best of our knowledge this has not been reported in the English literature so far and our case is the first such case.
Conclusion
Diverted TEF children on oral sham feeds have a voracious appetite. Clinicians should always think out of the box when the usual treatments for common conditions do not bring desired consequences. This is the first reported case of foreign body in the upper pouch of diverted TEF in the literature.
A strong suspicion of foreign body ingestion must be held in such children presenting with recurrent respiratory tract infections.