- Visibility 388 Views
- Downloads 69 Downloads
- Permissions
- DOI 10.18231/j.ijmpo.2021.017
-
CrossMark
- Citation
Clinicopathological profile of female genital tract malignancies reported at a tertiary care center in Northern India
- Author Details:
-
Syed Fiza Mustaqueem *
-
Syed Belal Hassan
-
Syed Shamshad Ahmad
Abstract
Background: The proportion of cancers of genital tract origin in females ranges from 22.4% to 55.8% in India; thus posing a major health problem. The first step in controlling the cancer burden in any population is to collect information about its salient features in that particular cohort of patients. This study was performed to ascertain the profile of female genital tract malignancies reported at our center regarding the relative frequency of involvement of various sites, age and symptoms at presentation and histological subtypes.
Materials and Methods: All the confirmed cases of female genital tract malignancies received in the Department of Pathology were studied for a period of 2 years from November 2008 to October 2010.
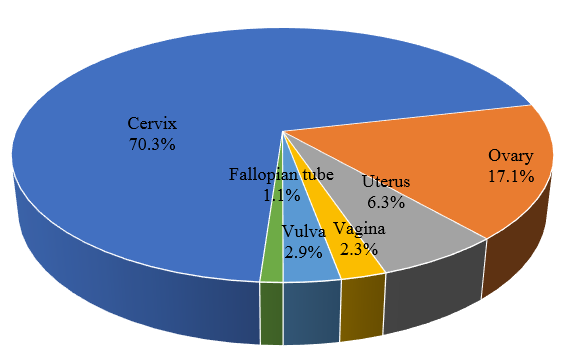
Result: A total of 175 cases were reported. The anatomic distributions were: cervix 123 (70.3%), uterus 11 (6.3%), ovary 30 (17.1%), vagina 4 (2.3%), vulva 5 (2.9%) and fallopian tube 2 (1.1%). The mean ages of women diagnosed with these cancers were: cervix (51.1 years), uterus (54.5 years), ovary (46.5 years), vagina (57 years), vulva (54.5 years) and fallopian tube (49.5 years). Women with cervical and uterine malignancies presented commonly with bleeding per vaginum; while those with ovarian malignancies presented mostly with abdominal mass. Women with vaginal and vulval malignancy presented with ulcers and masses. The most common histological subtypes at different sites were; Cervix: Squamous cell carcinoma (SCC) (87%); Uterus: Endometrioid adenocarcinoma (81.8%); Ovary: Serous cystadenocarcinoma (53.3%); Vagina: SCC (75%); Vulva: SCC (60%) and Fallopian tube (50% adenocarcinoma and 50 % metastatic carcinoma).
Conclusion: As female genital tract malignancies form a huge burden of morbidity and mortality in India, there is a need to establish better screening programmes aimed at early detection and educate the public regarding the risk factors as well as early symptoms of the disease so that people can adapt appropriate behaviour.
Introduction
Female genital tract (FGT) is the site of large number of tumours of considerable diversity, some very common and some extremely uncommon. However due to lack of cancer awareness and effective screening programmes in most developing countries including India, these malignancies constitute a major health burden.[1], [2] Also these tumours have dissimilar pattern of distribution and clinical presentation worldwide with ethnic, environmental and geographic variation. However the data relating to the clinicopathological characteristics of these tumours is deficient from Indian subcontinent indicating significant knowledge gap. An attempt is therefore made in the present study to assess the relative proportions and clinicopathological characteristics of FGT malignancies in our institution by a descriptive prospective histopathological study.
Materials and Methods
All cases reported at our center or referred to it and treated in the Department of Gynaecology over a period of 2 years were reviewed. The clinical data was collected from patient record files, discharge books and pathology request forms. From these data sources, age at diagnosis, clinical presentation at diagnosis, part of FGT affected and histopatholological characteristics were extracted. The data were entered into a computerized spreadsheet and analysis performed using Advanced Excel Sheet. Frequency distributions and descriptive statistics were calculated for each variable.
Results
Spectrum of FGT malignancies
A total of 175 cases of FGT malignancies were reported during the period under study. The anatomical distribution of these malignancies were: Cervix 123 (70.3%), Ovary 30 (17.1%), Uterus 11 (6.3%), Vagina 4 (2.3%), Vulva 5 (2.9%) and Fallopian tube 2 (1.1.%). Thus, cervix was the most common and fallopian tube the least common site of FGT malignancy in our study ([Table 1]).
|
Site of tumour |
No. of cases |
Percentage |
|
Cervix |
123 |
70.3 |
|
Ovary |
30 |
17.1 |
|
Uterus |
11 |
6.3 |
|
Vagina |
4 |
2.3 |
|
Vulva |
5 |
2.9 |
|
Fallopian tube |
2 |
1.1 |
|
Total |
175 |
100 |
Age distribution of various subtypes of FGT malignancies
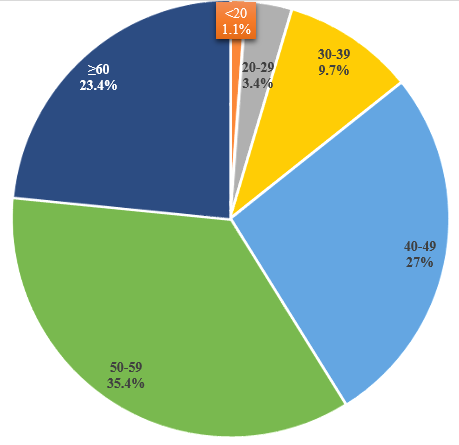
The ages of 175 women with FGT malignancies ranged from 10-69 years with a mean of 50.7 years. Majority of FGT malignancies (35.4%) were seen in the sixth decade, followed by 27 % cases in fifth decade and 23.4% cases in the seventh decade onwards. It was noted that the FGT malignancies were rare before the age of 20 years ([Table 2]).
|
Age group (years) |
No. of malignant cases |
Percentage |
|
<20 |
2 |
1.1 |
|
20-29 |
6 |
3.4 |
|
30-39 |
17 |
9.7 |
|
40-49 |
47 |
27 |
|
50-59 |
62 |
35.4 |
|
≥60 |
41 |
23.4 |
|
Total |
175 |
100 |
The ages of 123 women with malignancies of cervix ranged from 28-69 years with maximum number of cases 44(35.7%) in the age group of 50-59 years and a mean age of 51.1 years. The ages of 30 women with ovarian malignancies ranged from 18-65 years with maximum number of cases in the age group of 40-49 years and a mean age of 46.5 years. The ages of 11 women with malignancies of uterus ranged from 37-68 years with maximum number of cases 5(45%) in the age group of 60-69 years and a mean age of 54.5 years. The ages of 4 women with malignancy of vagina ranged from 55-67 years with maximum cases 3(75%) in the age group of 50-59 and a mean age of 57 years. The age of 5 women with vulval malignancy ranged from 48-68 years with maximum number of cases 3(60%) in the age group of 50-59 years and a mean age of 54.5 years. The age of 2 women with fallopian tube malignancy ranged from 47-56 years with 1 case each in the age group of 40-49 years and 50-59 years ([Table 3]).
|
Age group (years) |
Cervix |
Ovary |
Uterus |
Vagina |
Vulva |
Fallopian tube |
|
<20 |
0 |
2 |
0 |
0 |
0 |
0 |
|
20-29 |
3 |
3 |
0 |
0 |
0 |
0 |
|
30-39 |
13 |
2 |
2 |
0 |
0 |
0 |
|
40-49 |
35 |
9 |
1 |
0 |
1 |
1 |
|
50-59 |
44 |
8 |
3 |
3 |
3 |
1 |
|
≥60 |
28 |
6 |
5 |
1 |
1 |
0 |
|
Total |
123 |
30 |
11 |
4 |
5 |
2 |
Symptoms at presentation of FGT malignancies
Females with malignancies of cervix and endometrium commonly presented with bleeding per vaginum in 70 (56.9%) and 9 (81.8%) cases respectively. Females with ovarian malignancies commonly presented with abdominal mass in 15 (50%); vulval and vaginal malignancies with ulcer/mass 2(50%) and 3 (60%) respectively. 1 case of fallopian tube malignancy presented with abdominal mass and the other case was detected incidentally (Table 4).
|
Symptoms |
Cervix |
Endometrium |
Ovary |
Vagina |
Vulva |
Fallopian tube |
|
Bleeding per vaginum |
70 |
9 |
4 |
1 |
2 |
0 |
|
Vaginal discharge |
22 |
0 |
0 |
0 |
0 |
0 |
|
Ulcer/mass |
15 |
0 |
0 |
2 |
3 |
0 |
|
Abdominal mass |
0 |
0 |
15 |
0 |
0 |
1 |
|
Abdominal pain |
0 |
0 |
7 |
0 |
0 |
0 |
|
Menorrhagia |
4 |
2 |
2 |
0 |
0 |
0 |
|
Others |
2 |
0 |
2 |
1 |
0 |
1 |
Histological subtypes of FGT malignancies
The most common histological variant of malignancy at different sites were; Cervix - Squamous cell carcinoma (SCC) 87%, Ovary – Serous cystadenocarcinoma (53.3%), Uterus - Endometrioid carcinoma (81.8%), Vagina – SCC (75%) and Vulva – SCC (60%). 1 case each of adenocarcinoma and metastatic carcinoma were reported in fallopian tube ([Table 5]).
|
Site |
Histological type |
No. of cases |
Percentage |
|
Cervix |
Squamous cell carcinoma |
107 |
87 |
|
Adenocarcinoma |
11 |
8.9 |
|
|
Adenosquamous carcinoma |
2 |
1.6 |
|
|
Metastatic carcinoma |
3 |
2.4 |
|
|
Uterus |
Endometrioid adenocarcinoma |
9 |
81.8 |
|
Leiomyosarcoma |
1 |
9.1 |
|
|
Choriocarcinoma |
1 |
9.1 |
|
|
Ovary |
Serous cystadenocarcinoma |
16 |
53.3 |
|
Mucinous cystadenocarcinoma |
6 |
20 |
|
|
Dysgerminoma |
2 |
6.7 |
|
|
Yolk sac tumour |
1 |
3.3 |
|
|
Immature teratoma |
2 |
6.7 |
|
|
Granulosa cell tumour |
1 |
3.3 |
|
|
Metastatic carcinoma |
2 |
6.7 |
|
|
Vagina |
Squamous cell carcinoma |
3 |
75 |
|
Adenocarcinoma |
1 |
25 |
|
|
Vulva |
Squamous cell carcinoma |
3 |
60 |
|
Metastatic carcinoma |
2 |
40 |
|
|
Fallopian tube |
Adenocarcinoma |
1 |
50 |
|
|
Metastatic |
1 |
50 |
Discussion
During the period of 2 years under study, a total of 175 cases of FGT malignancies were diagnosed in our institution; out of which majority were from cervix (70.3%), followed by ovary (17.1%), uterus (6.3%), vulva (2.9%), vagina (2.3%) and fallopian tube (1.1%). This supports previous institutional based studies from other developing countries that found the commonest FGT malignancy to be cancer of uterine cervix.[3], [4], [5], [6], [7], [8] However the pattern of malignancy in our study differs from a study by Momtahen in Iran that showed a higher incidence of endometrial cancer (58%) and lesser prevalence of cervical cancer (13.6%).[9] The prevalence of cervical cancer in the current study, like in other developing countries has been attributed to the high prevalence of child marriage, early sexual activity, ignorance and lack of effective cancer screening programmes.
The mean age of women diagnosed with cancer of cervix was 51.9 years and maximum cases were in the age group of 50-59 years. However the data from Surveillance, Epidemiology and End Results Program of United States and European Union showed significantly higher proportion of cervical malignancies in the younger age group as compared to those reported at our center.[10] This may be a manifestation of better screening programmes in the US where cervical malignancy is detected in younger patients at a localized stage.
In the current study, the most common clinical presentation of women with carcinoma cervix was bleeding per vaginum; similar to other previous studies.[11], [12]
The most common histological subtype of cervical cancer was SCC (87%), followed by adenocarcinoma (8.2%) and adenosquamous carcinoma (1.6%). This was in concordance with the study of Shingleton et al [13] who has reported 83.8% cases of cervical carcinoma as SCC, 12.6 % as adenocarcinoma and 3.6% as adenosquamous carcinoma.
Ovary was the second leading site among FGT malignancies at our centre; constituting 17.1% of total FGT malignancies. This is in accordance with the data from Globocon 2002 which also shows a relatively higher incidence of ovarian malignancies in the West; similar to data from NCRP and other cancer registries in India.[14], [15], [16]
Most of the cases of ovarian malignancy occurred in the fifth decade and the mean age was 46.5 years. Yeole et al[17] have also reported maximum number of ovarian malignancies in the age group of 45-55 years.
The most common presenting complaint in cases of ovarian malignancy was lump in abdomen (80%), followed by pain in abdomen (73.3%). This corresponded with the findings of Maheshwari et al[18] who also found abdominal lump as presenting feature in 71.9% cases, followed by pain in abdomen in 47.4% cases.
Serous cystadenocarcinoma was the commonest malignant tumour of ovary in this study which accounted for 53.3% of malignant ovarian tumours. Katzenstein et al[19] found that that borderline and invasive tumours together constituted 35-40% of all malignant ovarian tumours.
In our study, carcinoma of uterine corpus was the third most common site of malignancy constituting 6.3% of all FGT malignancies. Jamal et al[20] also reported uterine malignancy to be the third most common amongst the gynaecological malignancies with an incidence of 16%.
Endometrial cancer is the cancer of post-menopausal females. The study showed maximum cases of endometrial carcinoma in the sixth decade and the mean age was 54.5 years. This was consistent with the findings of Jamal et al[20] who has reported the mean age of patients with endometrial carcinoma as 52.5 years.
The most common complaint of the patients of endometrial carcinoma in this study was abnormal uterine bleeding which was observed in 81.8% cases. Similar findings were reported by Hacker et al.[21]
Amongst the various histological subtypes of uterine malignancy, endometrioid adenocarcinoma was the most frequent type constituting 82% of all cases. Similar findings were observed by Platz et al[22] who reported it to be 81.5%.
Vagina, vulva and fallopian tubes were the less common sites of malignancy when compared to other sites of FGT. In the current study, the proportion of malignancy in these sites were reported to be 2.3%, 2.9% and 1.1% respectively of the total FGT malignancies. This finding suggests that cancer of vulva and vagina are not rare malignancies as determined in some studies.[23], [24] In the current study, fallopian tube (1.1%) was the least common site of malignancy in FGT. This differs from a study in Nigeria which reported vagina to be the least prevalent cancer of the FGT.[25]
The cases of vaginal, vulval and fallopian tube malignancy were reported in the fifth decade onwards. The mean age of diagnosis in vagina was 57 years, vulva 54.5 years and fallopian tube 49.5 years. This was in accordance with the findings of Jamal et al[20] who has reported these cases in the age group of 40-60 years.
Women with vaginal cancer and vulval cancer presented with ulcers and mass, similar to other studies. This differs from a study on vaginal cancer that reported bleeding per vaginum as the most frequent mode of presentation.[26]
In our study, squamous cell carcinoma constituted 60% cases of vulval and 75% cases of vaginal malignancy. This was in accordance with the findings of Platz et al[22] who also reported SCC to be the most common malignancy of vulva and vagina constituting 74.4% and 70.8% respectively.
In our study, 25% cases of vaginal malignancy were clear cell adenocarcinoma. Beller et al[27] have reported vaginal adenocarcinoma in 14% cases.
Both the cases of fallopian tube malignancy in this study were serous adenocarcinoma, one primary and the other metastatic. Baekelandt et al[28] have also reported serous adenocarcinoma as the most common malignancy of fallopian tube.
Conclusion
Although cancers of FGT are an important cause of morbidity and mortality among women worldwide; but there is significant lacunae in the FGT cancer detection programmes in India. So larger and more detailed study on the trends of FGT cancers is essential to plan better cancer detection strategies for specific age groups at risk.
Conflict of Interest
The authors declare that there are no conflicts of interest in this paper.
Source of Funding
None.
References
- Ferlay J, Shin HR, Bray F, Forman D, Mathers C. Estimates of worldwide burden of cancer in 2008: GLOBOCON. Int J Cancer. 2008;127:2893-917. [Google Scholar]
- . World Health Organization. World Cancer Report 2008. Lyon: International Agency for Research on Cancer . . 2008. [Google Scholar]
- Basile S, Angioli R, Manci N, Palaia I, Plotti F. Gynecological cancers in developing countries: the challenge of chemotherapy in low-resources setting. Int J Gynecol Cancer. 2006;16:1491-7. [Google Scholar]
- Mishra K. Gynecological malignancies from palliative care perspective. Indian J Palliat Care. 2011;17:45-51. [Google Scholar]
- Hanoon P, Nibedital B, Dhraba U. Malignancies of the female genital tract. J Obstet Gynaecol Cancer. 2007;2:35-8. [Google Scholar]
- FK, Jatoi N, Das C. Genital tract malignancies in post menopausal women. J Ayub Med Coll Abottabad. 2010;22:32-4. [Google Scholar]
- Mishra K. Gynaecological malignancies from palliative care perspective. Indian J Palliat Care. 2011;17:45-51. [Google Scholar]
- Nkyeker K. Pattern of gynaecological cancers in Ghana. East Afr Med J. 2000;77:534-8. [Google Scholar]
- Momtahen S, Kadivar M, Kazzazi AS, Gholipur F. Assessment of gynaecologic malignancies: a multi-center study in Tehran. Indian J Cancer. 1995;46:226-30. [Google Scholar]
- Bethesda M. Seer.cancer.gov. Bethesda, Maryland: North American Association of Central Cancer Registries; c2000. . 1975-2007. [Google Scholar]
- Hamad H. Cancer initiatives in Sudan. Ann Oncol. 2006;17:32-6. [Google Scholar]
- Kumar V, Abbas AK, Fausto N, Mitchell RN. Robbins Basic Pathology . 8th Edn.. 2007;8:718-21. [Google Scholar]
- Shingleton H, Bell M, Fremgen A, Chmiel J, Russell A, Jones W. There really a difference in survival of women with squamous cell carcinoma, adenocarcinoma and adenosquamous cell carcinoma of the cervix?. Cancer. 1995;76:1948-55. [Google Scholar]
- . Indian Council of Medical Research. Bangalore: National Cancer Registry Programme-2007. Consolidated Report of Hospital Based Cancer Registries. . 2001-2003. [Google Scholar]
- Chhabra S, Sonak M, Prem V, Sharma S. Gynaecological malignancies in a rural institute in India. J Obstet Gynaecol. 2002;22:426-9. [Google Scholar]
- Ferlay J, Bray F, Pisani P, Parkin D. GLOBOCON 2002: Cancer Incidence, Mortality and prevalence Worldwide. . 2004. [Google Scholar]
- Yeole B, Kumar A, Kurkure A, Sunny L. Population-based survival from cancers of breast, cervix and ovary in women in Mumbai, India. Asian Pac J Cancer Prev. 2004;5:308-15. [Google Scholar]
- Maheshwari V, Tyagi SP, Saxena K, Tyagi N, Sharma R, Aziz M. surface epithelial tumours of ovary. Indian J Pathol Microbiol. 1994;37:75-85. [Google Scholar]
- Katzenstein A, Mazur M, Morgan T, Kao M. Proliferative serous tumours of ovary: Histologic features and prognosis. Am J Surg Pathol. 1978;2:339-55. [Google Scholar]
- Jamal S, Mamoon N, Mushtaq S, Luqman M, Moghal S. The pattern of gynaecological malignancies in 968 cases from Pakistan. Ann Saudi Med. 2006;26:382-4. [Google Scholar]
- Hacker N. Practical Gynaecologic Oncology. 3rd Edn.. 2000. [Google Scholar]
- Ce P, Benda J. Female genital tract cancer. Cancer. 1995;75:270-94. [Google Scholar]
- Anderson E, Paavonen J, Murnaghan M, FT, PD. WHO Classification of Tumours No 4. Pathology and Genetics Tumours of the Breast and Female Genital Organs. . 2003. [Google Scholar]
- . Cancer Facts and Figures for 2009. American Cancer Society. . 2009. [Google Scholar]
- Ugwu EO, Iferikigwe ES, Okeke TC, Ugwu AO, Okezie OA, Agu PU. Pattern of gynaecological cancers in University of Nigeria Teaching Hospital. Niger J Med. 2011;20(2):266-9. [Google Scholar]
- . Vaginal Cancer. Gynaecologic malignancies 2005. Armenian Health Network, Health am. . . [Google Scholar]
- Beller U. Carcinoma of the vagina. Int J Gynaecol Obstet. 2003;83:27-39. [Google Scholar]
- Baekelandt M, Jorunn M, Kriestensen G, Trope C, Abeler V. Carcinoma of the fallopian tube. Cancer. 2000;89(10):2076-84. [Google Scholar]
How to Cite This Article
Vancouver
Mustaqueem SF, Hassan SB, Ahmad SS. Clinicopathological profile of female genital tract malignancies reported at a tertiary care center in Northern India [Internet]. IP Int J Med Paediatr Oncol. 2021 [cited 2025 Nov 06];7(2):85-89. Available from: https://doi.org/10.18231/j.ijmpo.2021.017
APA
Mustaqueem, S. F., Hassan, S. B., Ahmad, S. S. (2021). Clinicopathological profile of female genital tract malignancies reported at a tertiary care center in Northern India. IP Int J Med Paediatr Oncol, 7(2), 85-89. https://doi.org/10.18231/j.ijmpo.2021.017
MLA
Mustaqueem, Syed Fiza, Hassan, Syed Belal, Ahmad, Syed Shamshad. "Clinicopathological profile of female genital tract malignancies reported at a tertiary care center in Northern India." IP Int J Med Paediatr Oncol, vol. 7, no. 2, 2021, pp. 85-89. https://doi.org/10.18231/j.ijmpo.2021.017
Chicago
Mustaqueem, S. F., Hassan, S. B., Ahmad, S. S.. "Clinicopathological profile of female genital tract malignancies reported at a tertiary care center in Northern India." IP Int J Med Paediatr Oncol 7, no. 2 (2021): 85-89. https://doi.org/10.18231/j.ijmpo.2021.017
